Resources By Topic
Dementia 101
Learn how depression, anxiety, and stress can impact the onset and progression of dementia in older adults. This training explores the overlap between mental health conditions and dementia symptoms, the importance of accurate diagnosis, and practical strategies for early intervention and holistic dementia care. Ideal for caregivers, professionals, and anyone supporting older adults.
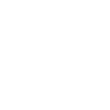
Dementia is the loss of cognitive functioning, the loss of the ability to think, remember, or reason, as well as loss of behavioral abilities, to an extent that it interferes with daily life. There are over 200 types of dementia, including neurodegenerative disorders, vascular dementia, and other conditions that can cause dementia-like symptoms. These disorders all fall under the “dementia umbrella.”
Research indicates that Black Americans are significantly more likely to develop Alzheimer's disease compared to other racial groups in the United States, with studies showing they are roughly 1.5 to 2 times more likely to be diagnosed with the disease than white Americans. Let’s learn why together.
Holidays shouldn’t stop just because of a dementia diagnosis! We have put together some tips and ideas to help everyone have a positive and joy-filled experience.
Frontotemporal dementia or FTD is a progressive disorder of the brain. It can can affect behavior, language skills and movement. Primary Progressive Aphasia (PPA)is one of the subtypes of FTD. Learn more about PPA, including the signs and symptoms, how it differs from other dementias, and the resources available locally and through AFTD.
It is back-to-school season, bringing fresh goals and aspirations for students and adults alike. However, for many, a dementia diagnosis complicates a dream of lifelong learning. Most people living with dementia can learn, and those that have trouble learning new skills can relearn a skill that had previously been acquired yet since forgotten. Learn more!
Financial planning is key when it comes to long-term care. With a diagnosis of dementia, the desire to stay at home is usually the first instinct, however, sometimes moving to a senior living community may make more sense. SEIA Client Services Director, Arvette M. Reid, shares some financial considerations.
Insight is excited to offer a new training opportunity focused on creating a dementia capable society! Dementia Capable Care (DCC) Training gives you the tools needed to be the best caregiver for those living at different stages of dementia. This training focuses on practical solutions to preventing and de-escalating behaviors, through online learning and an in-person session to address common scenarios.
We look at the importance of creating social circles in the LGBTQ community while navigating dementia. Being LGBTQ and living with dementia and/or caring for someone with dementia brings many unique challenges to the journey. Join us to discuss the importance of creating social circles of support and strategies for doing so. We will also identify community resources to support caring for someone living with dementia.
Around 3 million LGBTQ+ adults are over age 50, and those who receive a dementia diagnosis face a particularly challenging set of circumstances. Learn more about the services we offer as well as other national and local resources we have put together.
In the midst of summer, many of us reach for our favorite beach reads, looking forward to a few hours relaxing. If you’re looking to make the most of your summer reading list, here are a few recommendations that we and other care partners have found helpful.
Dementia does not discriminate - it affects people of all cultures and backgrounds. People’s backgrounds and beliefs inform their sense of self, how they understand, feel about, and respond to other people and their environment - including diagnoses, health and care organizations and their staff. It is important to know how to best provide care to meet one's needs while recognizing their cultural values and beliefs. Join us for an in-depth training on cultural specific care and how you can meet the person where they are with their needs.
It’s never too late or too early to incorporate healthy habits. Evidence shows when we incorporate these habits, we have a better chance of reducing cognitive decline. In recognition of Older Americans Month we are sharing 10 things you can do now to promote better brain health!
With concerns regarding the chronic use of pharmaceuticals and the peripheral damage it places on the human body with long-term use, CBD is presenting itself as possibly the overall best alternative for Alzheimer’s Dementia treatment because of its ability to mitigate further degradation of neuronal and synaptic damage. Adding CBD to your overall health and wellness as a preventative, potentially slowing the onset and progression of many disorders, could be a game changer for our aging community. Learn more!
Nearly half a million American veterans have Alzheimer’s — and as the population ages, that number is expected to grow. Veterans may be uniquely exposed to certain risk factors for Alzheimer’s and other dementias. We have compiled a list of resources that can provide information and assistance to both those diagnosed with dementia or Alzheimer’s disease or are caring for someone who has.
Navigating family dynamics can be tricky on a good day - but add in a dementia diagnosis and things get even more complex. Learn more about navigating these new dynamics!
By taking part in research, volunteers play a vital role in helping scientists understand more about the complex diseases that cause dementia. This means new ways to diagnose, prevent and treat these diseases can be developed and tested. Progress in dementia research just wouldn’t be made without the contributions volunteers make by participating in research. Learn more about the why and how of dementia research.
Supporting communication in the setting of dementia takes flexibility, creativity, and curiosity. A Speech Language Pathologist is a healthcare professional who specializes in evaluation and treating communication impairments, focusing on an individual’s strengths and personalized needs, with training for all communication partners. Through increased understanding of changing brain functions and development of proactive strategies, we can sustain meaningful connections, dignity, and respect in the face of this challenging condition.
Each year, Insight offers hundreds (yes hundreds!) of specialized classes for care partners to build their skills and confidence while learning more about new topics, services, and dementia resources in the community. Using our own dementia expertise and working with community partners for additional specialized topics, we're excited to continue to offer a wide variety of classes, workshops, trainings, author presentations, and even movie screenings in 2024. All of these sessions can be one more tool in your belt to being a stronger care partner! Check our full event calendar to see what's coming up!
Caring for a loved one with dementia poses many challenges for families and caregivers. People with dementia from conditions such as Alzheimer’s and related diseases have a progressive biological brain disorder that makes it more and more difficult for them to remember things, think clearly, communicate with others, and take care of themselves. In addition, dementia can cause mood swings and even change a person’s personality and behavior. We will look at practical strategies and medications (if needed) for dealing with the troubling behavior problems and communication difficulties often encountered when caring for a person with dementia.
Lewy body dementia is the second most common type of dementia, with an estimated 1.4 million Americans diagnosed. This October, in honor of Lewy Body Dementia Awareness Month, we've put together a few resources, both at Insight and in the wider community that may benefit your family.
What is frontotemporal degeneration (FTD)? Did you know it is the most common form of dementia for people under the age of 60? Learn more about FTD, including the signs and symptoms, how it differs from other dementias, and the resources available locally and through AFTD.
Summer 2023 has been marked by record breaking heat so far. In the midst of the summer season, it is crucial to highlight the significance of staying cool and hydrated, especially for older adults and individuals living with dementia. Learn some important information and tips to help keep older adults and those with dementia cool and comfortable this summer.
We can all use a helpful tip or two! Here are a few strategies that can be used to improve cognitive health and mental well-being for people living with Mild Cognitive Impairment (MCI) or dementia.
June is Brain Health Month! It’s never too late or too early to incorporate healthy habits. Evidence shows when we incorporate these habits, we have a better chance of reducing cognitive decline. Read on to learn more about cultivating habits to promote better brain health.
Our grief as caregivers can be so overwhelming. We may question ourselves “each day it feels like I am in persistent mourning, yet no death has occurred. I have lost loved ones to death before, so why now are my feelings as a dementia care partner so overwhelming?” Each day we may feel as if we are on a carousel of emotions - grief, loss, sadness, anger, joy, acceptance; a mixture of hope and despair, round and round we go. We must recognize the psychological impact of the ambiguous loss which accompanies our walk with our care person on this journey with dementia in order to begin to manage our unresolved grief.
Dementia, depression, and delirium can have many overlapping symptoms that can be hard to distinguish as a care partner. Both delirium and depression can cause cognitive changes that can easily be mistaken for dementia – but they can be treated differently to help your loved one significantly! Learn more about these 3 Ds and how to work with your physician to tell the difference.
When most people think of Parkinson’s disease, they think of a tremor. While movement symptoms are more noticeable, there are also cognitive changes that accompany the disease. During Parkinson's Awareness month, learn more and connect with resources from the Parkinson's Foundation.
April is Parkinson's Awareness Month! Learn more about resources and programs Insight offers that benefit families living with Parkinson's Disease, as well as download our Parkinson's resources handout for more info.
Dementia gradually diminishes a person’s ability to communicate. Communication with a person with dementia requires patience, understanding and good listening skills. Learn more about effective communication strategies in dementia care.
Around 3 million LGBTQ+ adults are over age 50, and those that receive a dementia diagnosis face a particularly challenging set of circumstances. Many, including care partners, face disproportionately high levels of social isolation and stigmatization as they age, making it difficult to find support. Join us to learn about resources and safe supports.
Health disparities can have a profound, negative effect on public health in the United States, entire populations and its individual communities. Dementia care and support services can vary widely depending on race, ethnicity, geography, and socioeconomic and political factors. The ability for a person to get a timely diagnosis, manage the disease, and be able to access quality health care contributes to health disparities in dementia. How can we learn and support change?
Lewy body dementias (LBD) affect an estimated 1.4 million individuals in the United States. Though many families are affected by this disease, few individuals and medical professionals are aware of the symptoms, diagnostic criteria, or even that LBD exists! The Lewy Body Dementia Association shares more about common symptoms, presentations of LBD, ways to live well going forward, and a resource list to learn more.
Using our own dementia expertise and working with community partners for additional specialized topics, we're excited to continue to offer a wide variety of classes, workshops, trainings, author presentations, and even movie screenings in 2023. All of these sessions can be one more tool in your belt to being a stronger care partner!
We all have that “hard to shop for” person in our family. You lean towards buying socks or gloves but choosing the perfect gift can be difficult or even impossible! What makes it even harder? If your loved one also has dementia. Here are some gift ideas for someone who has dementia, including options for those at the beginning to the end stages of the journey. Great gifts can provide the individual to have more autonomy and independence, or just simple joys and ways to relax. We hope these will be helpful!
In honor of Lewy Body Dementia Awareness month, Insight Memory Care Center, The Kensington Falls Church and The Kensington Reston held a special screening of the film SPARK. We learned more about Lewy Body Dementia through Robin William’s journey and afterwards had a great panel discussion with the Lewy Body Dementia Association. Here are your questions with their answers!
One of the most fascinating findings in studying human health and anatomy is how all of the systems in our body are inter-connected, and there have been recent studies done that have evidence to suggest that one of the most prominent connections is between our gut and our brain.
Have you heard the term “mild cognitive impairment?” If not, you are not alone. A recent survey of U.S. adults found that fewer than 1 in 5 Americans are familiar with mild cognitive impairment (MCI). Mild cognitive impairment is the stage between normal aging and dementia. While some cognitive changes are expected with age, individuals with MCI are experiencing more memory or thinking problems than other adults their age.
Dementia care is not one size fits all. Each person, each stage, and each family is unique. Come and learn about multiple care options to plan and evaluate what is right for your family.
How can you reconnect with someone with dementia? Keeping their current abilities in mind, learn ways to keep your loved one engaged in personalized activities.
In the midst of summer, many of us reach for our favorite beach reads, looking forward to a few hours relaxing. However, as a caregiver for someone with memory impairment, those relaxing moments can be few and far between – and the few you have, that time is valuable! If you’re looking to make the most of your summer reading list, here are a few recommendations that we and other care partners have found helpful.
Although LGBTQ+ older adults have clearly seen monumental change across their lifetimes and are often strong, determined, and resilient, many still struggle with complex feelings due to current and past experiences. When we take proactive steps to seek understanding, foster connection, and build trust slowly, we can make a huge impact on others and can create a world where LGBTQ+ individuals with dementia and their caregivers can feel safe and supported.
I recently had a dream that I was in my doctor's office being diagnosed with younger-onset Alzheimer's. I couldn't believe it, no matter how many times my spouse and my doctor told me it was true. I was so shocked and scared...more for my family would endure than for what was happening to me. Most dreams I forget within a few minutes of waking up. But not this one...it really hit home.
Have you ever considered your brain health could be related to what you are putting on your fork? There is evidence suggesting Alzheimer’s and other neurodegenerative diseases are highly influenced by diet, and are sometimes labeled Type 3 Diabetes. The mechanisms are elucidated in some research connecting diets high in sugar and processed food to inflammation which increases the risk of neurodegenerative diseases.
Researchers at the Johns Hopkins Center for Psychedelic and Consciousness Research in Baltimore, Maryland, are finding out! Scientists are studying the effects of psilocybin (a natural psychedelic found in some species of mushrooms) in people with depressed mood and a diagnosis of Early-Stage Alzheimer’s (AD) or Mild Cognitive Impairment (MCI).
The Inova Parkinson’s and Movement Disorders Center offers a variety of educational, wellness and supportive programs for patients, family and friends. In honor of Parkinson's Awareness month, they share some first steps to take upon a diagnosis of Parkinson's or a related memory disorder.
Over 15 years ago, Insight Memory Care Center developed a program designed for couples in the early stage of dementia find new ways to connect with each other, meet other families who are walking a similar path, focus on healthy minds and bodies, and adjust to life with a new diagnosis. The Mind & Body Workshop is often the first program families attend, many still nervous about joining a “memory loss” program. But the camaraderie of the group quickly turns anxieties into anticipation as families look forward to each next session.
With winter weather comes many things – a pretty dusting of snow, hot chocolate with marshmallows, and lots (and lots!) of indoor time. Freezing temperatures can easily make you go stir crazy, especially when trying to also care for and entertain a loved one with dementia. It’s easy to just default to watching TV all day, but by varying the types of activities you engage in, it really can still be the great indoors for everyone!
Looking for more information?
Contact Us!
Contact our Education Team at educate@insightmcc.org or 703-204-4664.