Blog
All Blog Posts
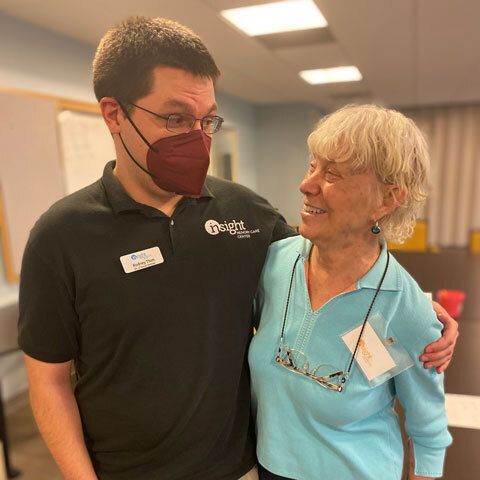
Insight is excited to offer a new training opportunity focused on creating a dementia capable society! Dementia Capable Care (DCC) Training gives you the tools needed to be the best caregiver for those living at different stages of dementia. This training focuses on practical solutions to preventing and de-escalating behaviors, through online learning and an in-person session to address common scenarios.
In the midst of the summer heat, it is crucial to highlight the significance of staying cool and hydrated, especially for older adults and individuals living with dementia. Here are a few tips to help keep older adults and those with dementia cool and comfortable this summer!
Summer is here, which for many of us means summer travel! Memory impairment adds a level of stress to taking a summer vacation, but whether you’re planning a day trip to visit family or a cross-country excursion, there are ways to minimize the anxiety. Here are a few tips to keep in mind for travel!
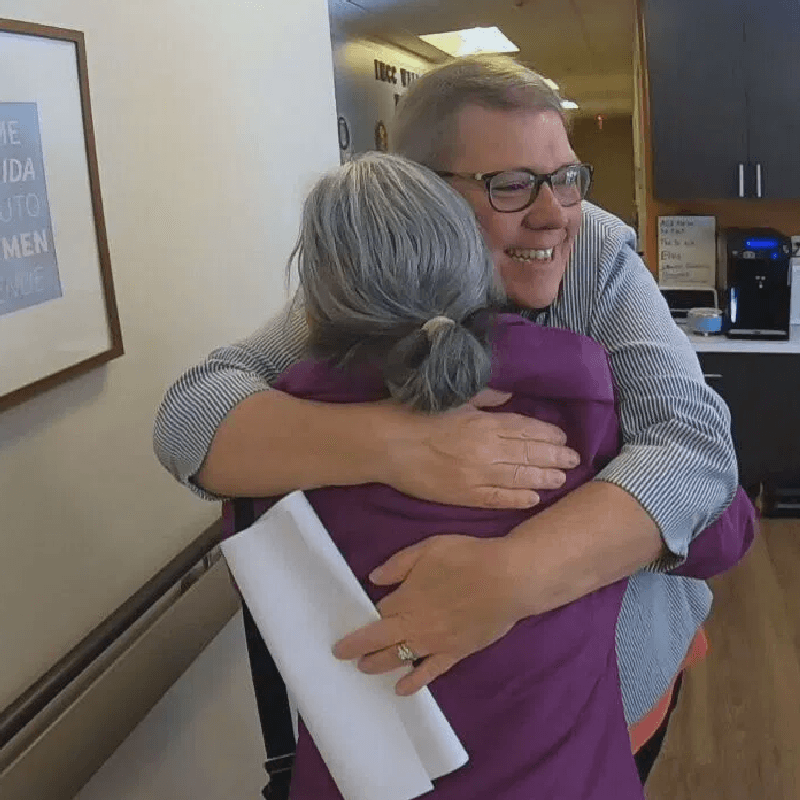
Melissa Long, our Director of Education and Support, was honored with a 2024 Equality Loudoun Pride Award for mission in service to the queer community and the Loudoun community! Melissa has made it her mission to be an ally to the LGBTQ+ community of Northern Virginia who are living with dementia. Her work aims to ensure that everyone with dementia feels comfortable seeking the resources they need to care for their loved ones safely and free from judgement. Congratulations, Melissa!
Many people have been to a café, and most are relatively familiar with the term memory – but have you heard of a memory café? Far from a restaurant that makes you memorize a long list of menu items, memory cafés are primarily social gatherings where individuals with memory impairment and their caregivers can join together in a safe, supportive environment, share conversation over a cup of coffee, or participate in fun, simple activities with the group. It’s an opportunity to meet with others for support, companionship, and fun - learn more!
Those hot summer days can feel longer without activities to keep busy and stay engaged! If you’re looking to make the most of the upcoming summer days in the DC Metro Area, check out this list of local dementia-friendly activities and outings we have put together.
Around 3 million LGBTQ+ adults are over age 50, and those who receive a dementia diagnosis face a particularly challenging set of circumstances. Learn more about the services we offer as well as other national and local resources we have put together.
In the midst of summer, many of us reach for our favorite beach reads, looking forward to a few hours relaxing. If you’re looking to make the most of your summer reading list, here are a few recommendations that we and other care partners have found helpful.
The opportunity to become a caregiver for a loved one can bring you closer and come with many positive experiences. However, it can also be challenging and overwhelming! You have to deal with everything from how to switch a reversed sleep schedule to finding meaningful activities to fill the day. In honor of Insight's 40th anniversary here are 40 top tips from our Caregiving at a Glance Guide - one for each year of Insight!
Dear Self, I have a job of being a caregiver. It is hard. It is an honor and privilege, but it can be very hard. I do not always feel like I am doing enough, can I do more? I must remind myself that I can only do what I am capable of. I do not know everything, nor can I physically do everything. Just because others think I can or need to do more, it does not mean that it’s right for me or my person...
You are on a journey that not everyone will travel, and your journey is unique. I wanted to share a letter I wrote to myself that I thought might be helpful to you.
It’s never too late or too early to incorporate healthy habits. Evidence shows when we incorporate these habits, we have a better chance of reducing cognitive decline. In recognition of Older Americans Month we are sharing 10 things you can do now to promote better brain health!
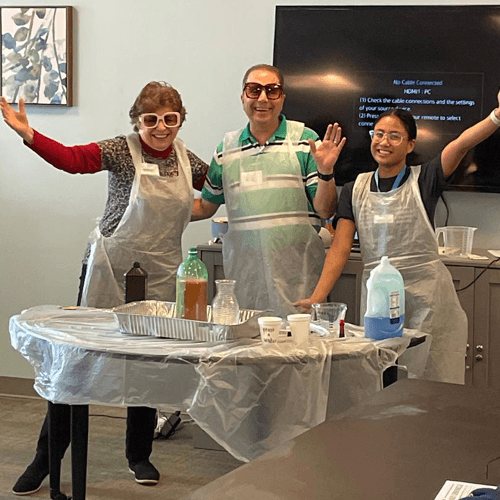
Recreational Therapy activities in Insight's Adult Day Center include cognitive, creative, physical, social, productive sensory, nature, outdoor, and reflective. Learn more!
In honor of National Volunteer Week, one of Insight’s newest volunteers shares more about her passions and why she volunteers to support those living with dementia. "Having experienced firsthand loving a family member who had Alzheimer's disease, I recognize it's a challenge that requires understanding, empathy, and, above all, awareness..."
With concerns regarding the chronic use of pharmaceuticals and the peripheral damage it places on the human body with long-term use, CBD is presenting itself as possibly the overall best alternative for Alzheimer’s Dementia treatment because of its ability to mitigate further degradation of neuronal and synaptic damage. Adding CBD to your overall health and wellness as a preventative, potentially slowing the onset and progression of many disorders, could be a game changer for our aging community. Learn more!
Nearly half a million American veterans have Alzheimer’s — and as the population ages, that number is expected to grow. Veterans may be uniquely exposed to certain risk factors for Alzheimer’s and other dementias. We have compiled a list of resources that can provide information and assistance to both those diagnosed with dementia or Alzheimer’s disease or are caring for someone who has.
Parkinson’s disease is a neurodegenerative disorder that affects predominately the dopamine-producing (“dopaminergic”) neurons in a specific area of the brain called substantia nigra. Symptoms typically develop slowly over the years, and often include tremors, slowness and paucity of movement, limb stiffness, and gait and balance problems. We've compiled a resource list of programs at Insight and offered in partnership with the Inova Parkinson’s and Movement Disorders Center that might be beneficial. Take a look!
We are grateful to have many talented social workers here at Insight who contribute to the organization in numerous positive ways and bring their social work mindset to each new or challenging situation. Whether it is connecting personally with participants, coordinating resources for families, engaging with the larger community, helping keep things going behind the scenes, or just being a listening ear, our social workers do extraordinary work to further our mission. As we celebrate Social Work Month - get to know a few of our social workers!
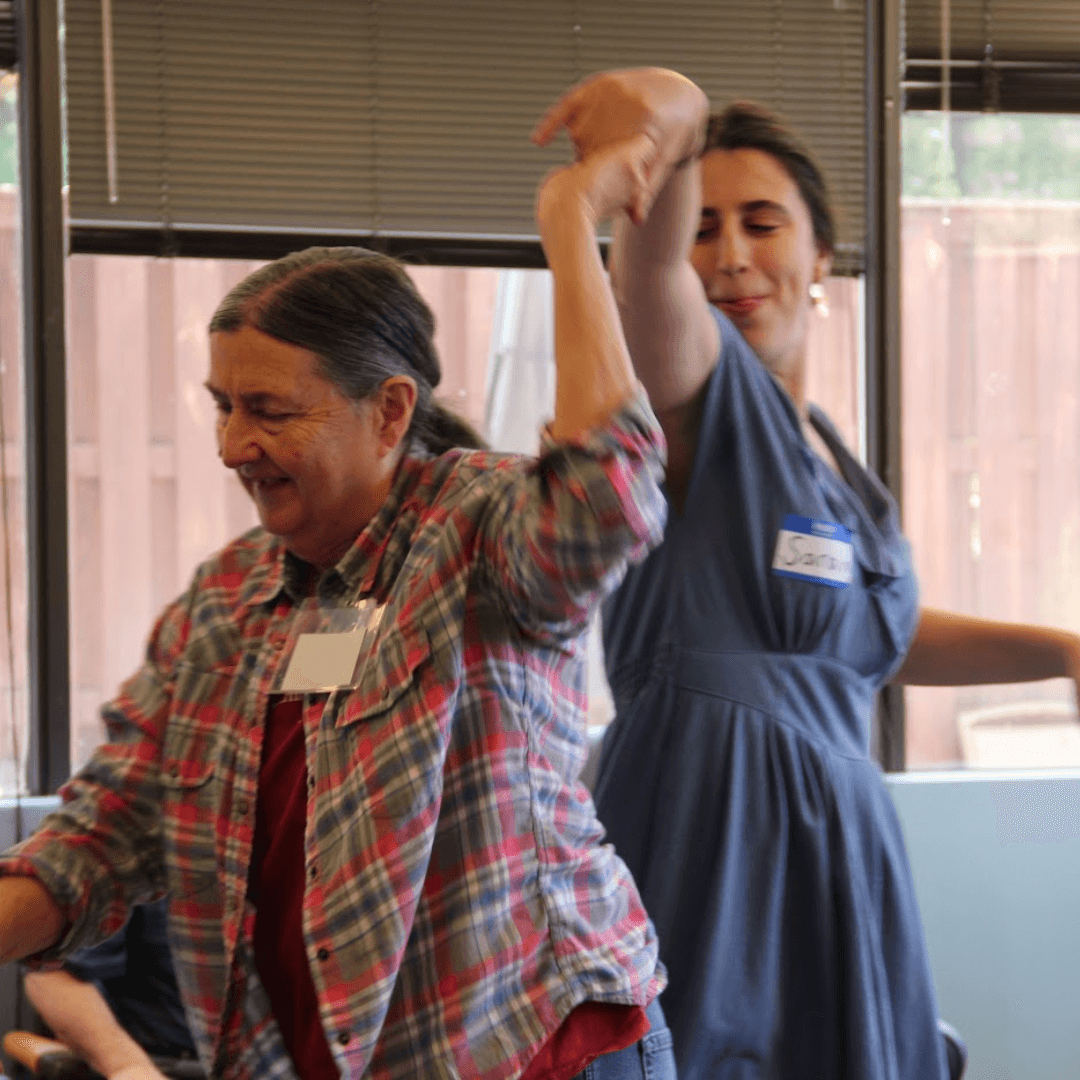
Research shows that the areas of the brain that control memory and skills such as planning and organizing improve with exercise. Dance has the added dimensions of rhythm, balance and music that enhance the benefits of simple movement. “Dance for Brain Health Classes” have started at the Workhouse Arts Center, Art of Movement in Lorton, and are beneficial for anyone experiencing cognitive decline as well as those interested in prevention!
According to the Bureau of Justice Statistics National Crime Victimization Survey, in 2014, 2.6 million persons over age 65 were victims of identity theft. Learn more about how it happens, signs to look for, how to avoid financial abuse, and what to do next if it does happen to you.
Insight Memory Care Center may be celebrating our 40th this year, but we also have another milestone anniversary on the horizon. This spring marks the 10th Anniversary of our Early Stage Reconnections program! We are so grateful that Reconnections has grown so much over the past 10 years, serving hundreds of individuals over its history.
Supporting communication in the setting of dementia takes flexibility, creativity, and curiosity. A Speech Language Pathologist is a healthcare professional who specializes in evaluation and treating communication impairments, focusing on an individual’s strengths and personalized needs, with training for all communication partners. Through increased understanding of changing brain functions and development of proactive strategies, we can sustain meaningful connections, dignity, and respect in the face of this challenging condition.
Our Early Stage Reconnections program builds community in Fairfax, Sterling, Alexandria, and online; Insight is so lucky to have an amazing team of recreation staff leading a variety of activities at each program. Whether it’s a lively reminiscence discussion, cornhole trivia, or an artist spotlight, our rec team provides engagement for each participant based on their interests and abilities. As we celebrate Recreation Therapy month, meet the early stage team!
Insight is fortunate to have amazing recreation staff leading participants in a variety of activities each day. Whether it’s brain fitness, a new art project, music therapy, or interacting with technologies like the multi-sensory room, the Obie, or virtual reality, our rec team provides engagement and support to participants in all stages of their dementia journey. As we celebrate Recreation Therapy Month, learn more about our day center recreation team and hear what they admire about each other!
Around 3 million LGBTQ+ adults are over age 50, and those that receive a dementia diagnosis face a particularly challenging set of circumstances. Many, including care partners, face disproportionately high levels of social isolation and stigmatization as they age, making it difficult to find support. We have compiled a list of resources and safe supports, both national and local to the DC Metro Area & Virginia.
You’ve completed the intake assessment, squared away the physical paperwork, and signed all of the enrollment forms. Your loved one’s first day at the day center is on the calendar! But now you're wondering: What will the day look like? How will my loved one do?
We know that balance and strength training can decrease fall risk in older adults. Insight staff members have recently been trained in the Otago Exercise Program, a balance and strength training program which, if performed consistently, has been shown to decrease fall risk in older adults of 35 to 40 percent!
We are excited to announce that this year is our 40th anniversary! This incredible milestone marks four decades of unwavering commitment to providing quality dementia-specific care, support, and education in the Northern Virginia community. Here's a sneak peek at what's in store!
"Home care" and "Home health" are often used interchangeably, leading to confusion among families seeking the most appropriate support for their loved ones. While both services aim to enhance the well-being and independence of individuals in their homes, they differ significantly in their scope, focus, and requirements. Understanding these distinctions is crucial for making informed decisions that align with the specific needs of the individual. Read on to learn more!
It seems as though everyone makes New Year’s resolutions – eat healthy, clean out the house, exercise more, the list could go on and on. And despite our best intentions, these resolutions are usually out the window before we’ve even turned the calendar over to February. However, resolutions can be a great way to start off the New Year when you can keep them! Here are 5 resolutions for care partners that you can actually keep!
Each year, Insight offers hundreds (yes hundreds!) of specialized classes for care partners to build their skills and confidence while learning more about new topics, services, and dementia resources in the community. Using our own dementia expertise and working with community partners for additional specialized topics, we're excited to continue to offer a wide variety of classes, workshops, trainings, author presentations, and even movie screenings in 2024. All of these sessions can be one more tool in your belt to being a stronger care partner! Check our full event calendar to see what's coming up!
In Parts 1 – 6, I mentioned issues that Marie and I faced as we proceeded on this journey and I discussed the options we used to address them or overcome obstacles. Since we did not use every option available to us to take care of problems/needs as they arose and to give you a broader knowledge of the help that is available to you in caring for your loved one, we have compiled some resources and information that you may find helpful.
The holiday season often brings feelings of "guilt" for care partners. However, as we begin to be curious about these feelings of guilt, we begin to see this as something more than guilt - we begin to uncover grief, masquerading as guilt. Guilt and grief are both powerful human emotions, it is essential to understand their differences.
“I did a lot of interaction in my previous life, and I just like being around people. And when I wasn't doing that, it just depressed me,” shares Rick, a participant in our early stage Reconnections program. Lindsey Vajpeyi, Director of Early Stage Programs, elaborates, "At Insight, people find a community. They find others who are going through something like they are and really get it." Watch their stories.
As winter is upon us you may find yourself with extra free time home for the holidays, stuck inside due to the weather, or both! If you’re looking to make the most of this season while spending more time inside, we have compiled a list of virtual activities and programs you can access from the comfort of home to help your loved one stay engaged.
The holiday season is a time of new and old traditions, and sharing in the joy and togetherness of spending time with friends and family. But for families whose loved ones are diagnosed with Alzheimer’s or dementia, the holidays can be stressful and overwhelming; and for family care partners, often difficult to remember the joy that holidays can bring. We have put together some tips to help you experience this holiday season even with some new challenges.
Tuesday, November 28th was Giving Tuesday, a worldwide day of giving! You’ve probably heard of Black Friday, Small Business Saturday, and Cyber Monday as shopping days – Giving Tuesday is day to celebrate giving! But it's not just a day for us to ask for your support - we wanted to give back too! We had a great time celebrating on Facebook, LinkedIn, and YouTube - sharing resources, caregiving tips, advice, and stories.
Here are some gift ideas for someone who has dementia, including options for those at the beginning to the end stages of the journey. Great gifts can provide the individual to have more autonomy and independence, or just simple joys and ways to relax. We hope these will be helpful!
Holidays shouldn’t stop just because of a dementia diagnosis! If you’re visiting a loved one with memory loss, the holidays can be poignant, awkward, funny, and everything else. Here are a couple of ideas to help ensure they are also a positive and joy-filled experience!
"Insight is not your typical place. You know, at Insight, they treat the individual as an individual," shares Mary, care partner for her husband. Hear more as Mary shares their story.
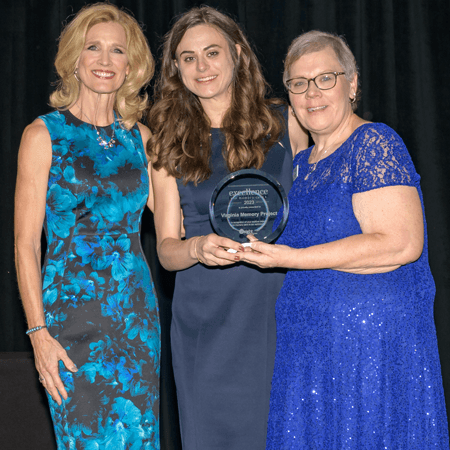
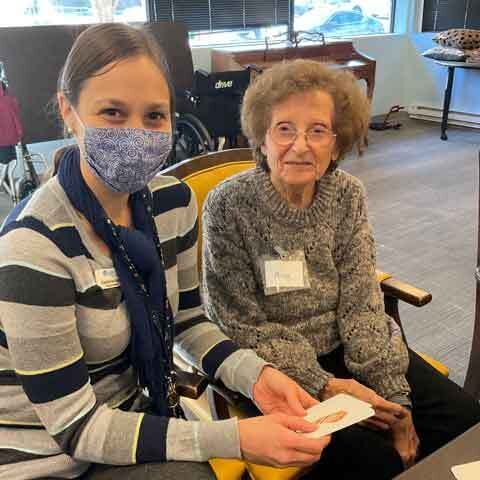
Insight Memory Care Center’s Excellence in Memory Care Award recognizes programs and services that are models of excellence and are positively impacting memory care in our community. Congratulations to our 2023 winner, Annie Rhodes and the Virginia Memory Project team! We sincerely thank you for your impact on memory care across all of Virginia! Read on to learn more about the work of the Virginia Memory Project.
FAIRFAX, Va. (7News) — A Fairfax County non-profit that’s called a lifeline for families and patients with memory-robbing dementia held a gala fundraiser Friday night. The dictionary defines insight as a clear perception. But for these folks, insight is a very real, very tangible place. Insight Memory Care Center offers help for both the patient and the family on a journey that rarely has a happy ending. "There is nothing more gratifying than working for an organization that can create those quality moments for such an insidious disease," Anita Irwin...
It's no secret that the worlds of healthcare and memory care can be full of confusing acronyms. While acronyms can help make communication more concise, a conversation full of them can also feel as if you are on the outside and unable to keep up! We have compiled a list of common acronyms you may come across as a care partner and what they mean.
Lewy body dementia is the second most common type of dementia, with an estimated 1.4 million Americans diagnosed. This October, in honor of Lewy Body Dementia Awareness Month, we've put together a few resources, both at Insight and in the wider community that may benefit your family.
Insight Memory Care Center’s Excellence in Memory Care Award recognizes programs and services that are models of excellence and are positively impacting memory care in our community. The 8th Annual Award will be presented at the event on October 20th. This year we have three fantastic finalists. The winner will be announced the evening of the event. Learn more about our finalists and the impactful work they are doing!
We are excited to share that Jennifer Denk, our Director of Community Engagement, has been appointed the Fairfax Village in the City Advisory Board, where she will serve as a subject matter expert on dementia! The Advisory Board is composed of 9 to 15 city residents representing key stakeholder groups; Jen will be able to share dementia expertise and bring awareness for those living with dementia looking to age in place in their Fairfax City community.
Receiving an Alzheimer's or dementia diagnosis is daunting enough, but navigating all the options for care can quickly become even more overwhelming. One option that many have never heard of? Adult Day Programs. While we might be a bit biased here at Insight, we believe that day centers and day programs can be the perfect happy medium for many families - support, engagement, and safety during the day, and the comforts of family and home in the evening. In honor of National Adult Day Services Week, here are a few reasons to consider a day program.
Adult Day Services Week is a special week that has been celebrated annually since it was proclaimed in 1983 by former President Ronald Reagan. The third complete week of September is set aside to raise awareness of the availability and accessibility of adult day programs nationwide. If you’re familiar with Insight, you might already know this, but first what are Adult Day Services?
It’s important to gather as much information from your doctor as you can. Asking the right questions can help you navigate your appointments and this journey. Check out a neuropalliative specialist's recommended list of questions to ask your neurologist.
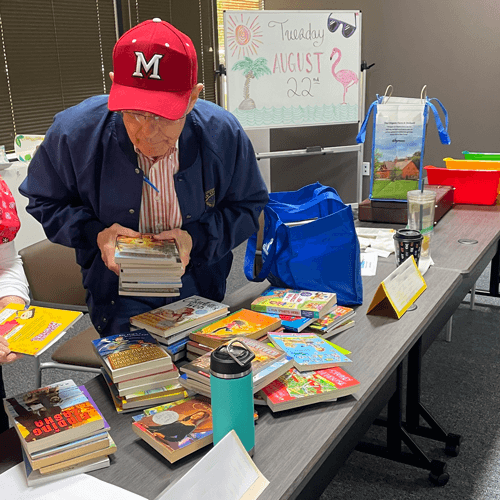
Reconnections has partnered with local Loudoun County non-profit, By Faith Fund, several times over the past year on donation drives for needs in the community including food, toiletries, holiday items, and school supplies. Most recently participants and their families had the opportunity to participate in a school supply and backpack drive for local students as the school year begins!
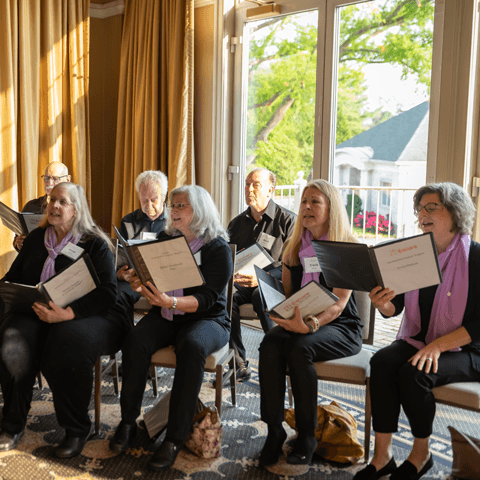
Encore Creativity for Older Adults is the nation’s largest choral organization with 42 ensembles in 7 states and the District of Columbia, serving almost 1300 singers. Sentimental Journey Singers, offered at Insight - Fairfax and Insight - Sterling is a FREE program for Insight participants and care partners to participate in. Come sing, laugh, and play with us at Insight!
Those hot summer days can feel longer without activities to keep busy and engaged. If you’re looking to make the most of the remaining summer days in the DC Metro Area, check out this list of local dementia-friendly activities and outings we have put together.
Insight completes an annual survey each spring, asking all of our participants, care partners, and families to provide their feedback on all of our programs. Here is what our families had to say over this past fiscal year, July 2022 to June 2023.
Making the “right” choice when it comes to where you choose to live can be difficult. Learn more about the process of rightsizing and things to keep in mind when considering finding a new space to live for your stage of life.
In the midst of summer, many of us reach for our favorite beach reads, looking forward to a few hours relaxing. However, as a caregiver for someone with memory impairment, those relaxing moments can be few and far between – and the few you have, that time is valuable! If you’re looking to make the most of your summer reading list, here are a few recommendations that we and other care partners have found helpful.
As we take a look back over the past year, here's a little bit about what we've been up to and what we were able to accomplish over the last year, from July 2022 to June 2023!
Summer 2023 has been marked by record breaking heat so far. In the midst of the summer season, it is crucial to highlight the significance of staying cool and hydrated, especially for older adults and individuals living with dementia. Learn some important information and tips to help keep older adults and those with dementia cool and comfortable this summer.
Caring for a loved one with Alzheimer's or dementia can be all-consuming and any focus on self-care often shifts to ensuring our loved one’s needs are met first. It takes courage to ask for and accept help. Yet, asking for help is often a starting point on the journey of self-care. This care extends to our own healing as we grieve the loss of our loved one. The support of others, including Insight Memory Care, can be sustaining.
We can all use a helpful tip or two! Here are a few strategies that can be used to improve cognitive health and mental well-being for people living with Mild Cognitive Impairment (MCI) or dementia.
One concept that it took me some time to ‘get,’ is that it’s important to recognize that although your loved one isn’t who they used to be, both cognitively and emotionally, they continue to need to be treated with dignity and to have friendships and a life of their own. This is especially the case, since they are no longer living with you 24/7. It doesn’t mean that they don’t love you, it simply reflects a recognition that your living situation has changed.
Summer is here, which for many of us means summer travel! Memory impairment adds a level of stress to taking a summer vacation, but whether you’re planning a day trip to visit family or a cross-country excursion, there are ways to minimize the anxiety. Here are a few tips to keep in mind for travel.
June is Brain Health Month! It’s never too late or too early to incorporate healthy habits. Evidence shows when we incorporate these habits, we have a better chance of reducing cognitive decline. Read on to learn more about cultivating habits to promote better brain health.
Despite all of the care, assistance, and precautions, this was the third ambulance ride Marie had had due to a fall in the past four months. It was this last fall that convinced me that the most important thing to be considered was not my need to take care of Marie at home, but what was best for Marie.
A big part of engaging in our programs is actually getting to the programs! You are of course welcome to provide your own transportation, but we know this may not work for every family situation. Here are a few door-to-door transportation options available in Northern Virginia to get here safely.
The Cadette and Junior Girl Scouts from Troop 53039 in Alexandria, VA recently completed a wonderful service project at the Insight Fairfax day center location. The project involved painting flowerboxes, planting flowers, and cleaning an outdoor sensory space for the participants.
When they first came to Insight, they were in search of ways to stay engaged after a new diagnosis (and extended time at home during COVID!). What they found was a supportive environment for both of them. Monica shares, “He’s very happy here. I know he is. Because he wants to come.” Hear more as Monica shares their story.
Our nursing team goes above and beyond to care for our participants everyday. Not only do they keep our participants at the day center healthy and safe, they also prioritize creating relationships with all participants and putting in the effort to ensure that each one of our participants feels welcome and valued. We are very grateful to have this compassionate and dedicated team as part of our Insight family. As we recognize National Nurse's Week, meet our fabulous nursing team!
Our grief as caregivers can be so overwhelming. We may question ourselves “each day it feels like I am in persistent mourning, yet no death has occurred. I have lost loved ones to death before, so why now are my feelings as a dementia care partner so overwhelming?” Each day we may feel as if we are on a carousel of emotions - grief, loss, sadness, anger, joy, acceptance; a mixture of hope and despair, round and round we go. We must recognize the psychological impact of the ambiguous loss which accompanies our walk with our care person on this journey with dementia in order to begin to manage our unresolved grief.
Making important decisions for aging parents can be a challenging task, but Power of Attorney (PoA) can provide peace of mind and clarity in times of need. This article from Legacy Lawyers, PLLC will walk you through the different types of PoAs, why and when to consider a PoA, and how to choose a PoA.
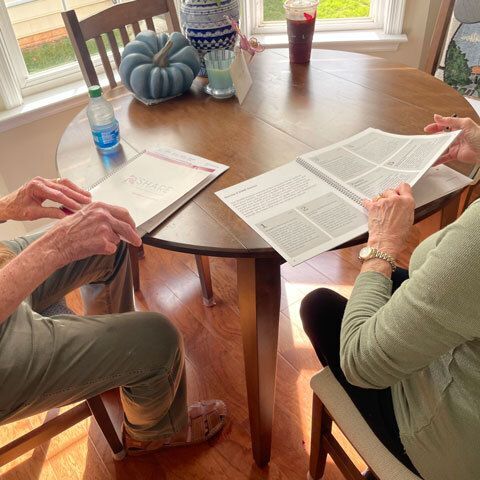
“We have recently participated in and completed the SHARE for Dementia program. We found it to be an invaluable resource and tool to plan for and prepare ourselves and our family for the inevitable changes and issues that lie ahead. We were initially reluctant to address topics that might increase our fear of future challenges, however our counselor, Melissa Long, guided us through the SHARE platform skillfully and provided us with a level of comfort that allowed us to walk through the process with ease and a growing confidence that we were making the best possible plans for our future.”
When most people think of Parkinson’s disease, they think of a tremor. While movement symptoms are more noticeable, there are also cognitive changes that accompany the disease. During Parkinson's Awareness month, learn more and connect with resources from the Parkinson's Foundation.
April is Parkinson's Awareness Month! Learn more about resources and programs Insight offers that benefit families living with Parkinson's Disease, as well as download our Parkinson's resources handout for more info.
Mark your calendar for these upcoming events with Insight! We have many great events scheduled this spring, check out the blog to learn more. We look forward to having you join us for some or all of these events!
Did you know that today is National Doctor's Day? Our doctors work hard to provide quality care for their patients,
including when they start to see changes in memory. If you're noticing changes in your memory, make your next visit easier for your doctor! Here’s what to bring, what to expect, and some questions to ask at your visit.
Social workers play a variety of roles in organizations across the country. Here at Insight Memory Care Center, our social workers impact the lives of participants and families in numerous positive ways. As we celebrate National Social Work Month, we honor the critical role Insight’s social workers play in our organization and the greater community!
We are grateful to have many fabulous social workers here at Insight who contribute to the organization in a variety of ways. Whether it is connecting with participants, coordinating resources for families, engaging the community, or just being a listening ear, our social workers do extraordinary work to further our mission. As we celebrate Social Work Month, meet our social workers!
Since I had been taking care of Marie’s increasing needs as the disease progressed, I decided that the best course of action at that time was just to continue doing what we were doing. Besides, not being a member of the health care community, I didn’t know of any other options. So for the time being, we would go it alone. After all, I reasoned, who can better take care of your loved one than you?
Dementia gradually diminishes a person’s ability to communicate. Communication with a person with dementia requires patience, understanding and good listening skills. Learn more about effective communication strategies in dementia care.
Insight is fortunate to have an amazing recreation staff leading participants in a variety of activities each day. Whether it’s brain fitness, a new art project, music therapy, or interacting with technologies like the multi-sensory room, the Obie, or virtual reality, our rec team provides engagement and support to participants in all stages of their dementia journey. As we celebrate Recreation Therapy Month, meet the rec team!
As our Early Stage Reconnections program has expanded to Fairfax, Sterling, and virtual options, Insight is so lucky to have an amazing team of recreation staff leading a variety of activities at each program. Whether it’s a lively discussion, cornhole trivia, an artist spotlight, or a virtual program with the Smithsonian, our rec team provides engagement for each participant based on their interests and abilities. As we celebrate Recreation Therapy month, meet the early stage team!
One of the top questions we get about our programs at Insight is “what do they do all day?” It’s a natural question, since many of us have images of seniors playing bingo all day in our heads! At Insight Memory Care Center, we work hard to ensure that participants are engaged in a wide variety of activities at all levels of our programs – which is where we depend on our fantastic recreation therapists!
Insight Memory Care Center is excited to begin a virtual reality program – the first of its kind – to boost engagement, mental wellness, and quality of life for senior participants in our adult day health center. Anita Irvin, Executive Director, shares, “We are always looking for innovative ways to engage our participants in our day programs. When we were first looking at the option of virtual reality, our staff was quickly on board when we realized all the possibilities for our participants to reminisce, connect, and engage with each other in new ways."
Around 3 million LGBTQ+ adults are over age 50, and those that receive a dementia diagnosis face a particularly challenging set of circumstances. Many, including care partners, face disproportionately high levels of social isolation and stigmatization as they age, making it difficult to find support. Watch our recent webinar at take a look at the resource listing!
Health disparities can have a profound, negative effect on public health in the United States, entire populations and its individual communities. Dementia care and support services can vary widely depending on race, ethnicity, geography, and socioeconomic and political factors. The ability for a person to get a timely diagnosis, manage the disease, and be able to access quality health care contributes to health disparities in dementia. How can we learn and support change?
Marie had an appointment with a neurologist, who gave her a diagnosis of dementia, most likely Alzheimer’s Disease. Marie was totally unfazed by it. I wish I could say the same for myself. All the way home from the appointment, I kept repeating to myself, “what do we do now?,” “what do we do now?”
Lewy body dementias (LBD) affect an estimated 1.4 million individuals in the United States. Though many families are affected by this disease, few individuals and medical professionals are aware of the symptoms, diagnostic criteria, or even that LBD exists! The Lewy Body Dementia Association shares more about common symptoms, presentations of LBD, ways to live well going forward, and a resource list to learn more.
"My hope for Insight in the future is that we continue to serve our home base here, but at the same time expand our reach further and further," shares Rodney. "My own grandmother, she was diagnosed with dementia. She lives in North Carolina and she doesn't have stuff like this there," says Selena. Listen as staff and family members share their hopes for the future with Insight Memory Care Center.
It seems as though everyone makes New Year’s resolutions – eat healthy, clean out the house, exercise more, the list could go on and on. And despite our best intentions, these resolutions are usually out the window before we’ve even turned the calendar over to February. However, resolutions can be a great way to start off the New Year when you can keep them! Here are 5 resolutions for care partners that you can actually keep!
Using our own dementia expertise and working with community partners for additional specialized topics, we're excited to continue to offer a wide variety of classes, workshops, trainings, author presentations, and even movie screenings in 2023. All of these sessions can be one more tool in your belt to being a stronger care partner!
We all have that “hard to shop for” person in our family. You lean towards buying socks or gloves but choosing the perfect gift can be difficult or even impossible! What makes it even harder? If your loved one also has dementia. Here are some gift ideas for someone who has dementia, including options for those at the beginning to the end stages of the journey. Great gifts can provide the individual to have more autonomy and independence, or just simple joys and ways to relax. We hope these will be helpful!
“Stephen had undiagnosed probable Lewy Body dementia and he took cold tablets, which can set the disease process in full blown proportions. And that’s how we started with Lewy Body – jumped in with both feet,” shares Lynn, care partner for her husband. Watch their story.
Tuesday, November 29th is Giving Tuesday, a worldwide day of giving. You’ve probably heard of Black Friday, Small Business Saturday, and Cyber Monday as shopping days – Giving Tuesday is day to celebrate giving! We celebrated live on Facebook, LinkedIn, and YouTube all day – sharing resources, caregiving tips, advice, and stories. Check out the panels and presentations!
Tuesday, November 29th is Giving Tuesday, a worldwide day of giving! You’ve probably heard of Black Friday, Small Business Saturday, and Cyber Monday as shopping days – Giving Tuesday is day to celebrate giving!
This diagnosis was rendered about five years following Marie’s car accident. At the beginning of that time, we had been wondering if there was something going on, and at the end of it we were wondering just what was going on. Despite the time frame and all of the wondering, thinking, and reading about the possibilities, the diagnosis was still a shock. Essentially, we knew that something was wrong, and just what was wrong now had a name.
If you had a disease such as Alzheimer’s affecting your brain, would you want to know? If so, when would you want to know? If not, why not? Studies show us that this is a complicated question!
In honor of Lewy Body Dementia Awareness month, Insight Memory Care Center, The Kensington Falls Church and The Kensington Reston held a special screening of the film SPARK. We learned more about Lewy Body Dementia through Robin William’s journey and afterwards had a great panel discussion with the Lewy Body Dementia Association. Here are your questions with their answers!
One of the most fascinating findings in studying human health and anatomy is how all of the systems in our body are inter-connected, and there have been recent studies done that have evidence to suggest that one of the most prominent connections is between our gut and our brain.
Have you heard the term “mild cognitive impairment?” If not, you are not alone. A recent survey of U.S. adults found that fewer than 1 in 5 Americans are familiar with mild cognitive impairment (MCI). Mild cognitive impairment is the stage between normal aging and dementia. While some cognitive changes are expected with age, individuals with MCI are experiencing more memory or thinking problems than other adults their age.
We are sincerely grateful to Home Instead for being a Diamond Sponsor of our 2022 Paintings & Pairings event! Just like Insight, they believe strongly in the value of compassionate care for those living with dementia. Learn more!
We are sincerely grateful to Retirement Unlimited, Inc. for being a Diamond Sponsor of our 2022 Paintings & Pairings event! Just like Insight, they believe strongly in the value of education and lifelong learning. Learn more about their RUI University!
I am a gay woman in my late 70’s. My partner and I were together for over 40 years. About ten years ago, Marie began experiencing unusual events; first a broken leg, and then a car accident a year later. After that, things settled down for a while; or at least they seemed to. As it turned out, Marie was quite adept at hiding her memory issues; and I appeared to have missed what, to some of Marie’s friends, was obvious. She was becoming forgetful.
Blog
"I like that IMCC focuses on dementia-related problems and provides a focal point for families to network and socially interact in coping with dementia. It provides a community that helps us in our struggle."